Primary Criteria
Primary Criteria - Mandatory selection to identify patients based on either Diagnosis / Treatment (NDC) / Procedure / Surgery Events. The outcome of Primary Criteria will be Patient Id and Index Date, it will be unique at Patient Id.
Events -
Diagnosis Event – It will fetch patients based on Diagnosis Codes ICD10CM / ICD9CM
Treatment Event – It will fetch patient based on NDC Codes (Treatment of Interest) and Procedure of Interest (Optional) CPT/HCPCS/ICD10PCS/ICD9PCS
Procedure Event - It will fetch patient based on Procedure of Interest CPT/HCPCS/ICD10PCS/ICD9PCS
Surgery Event - It will fetch patient based on Procedure of Interest CPT/HCPCS/ICD10PCS/ICD9PCS
*1*.One Individual Event
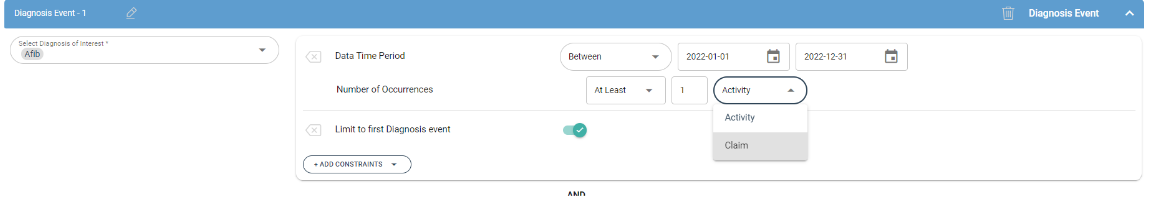
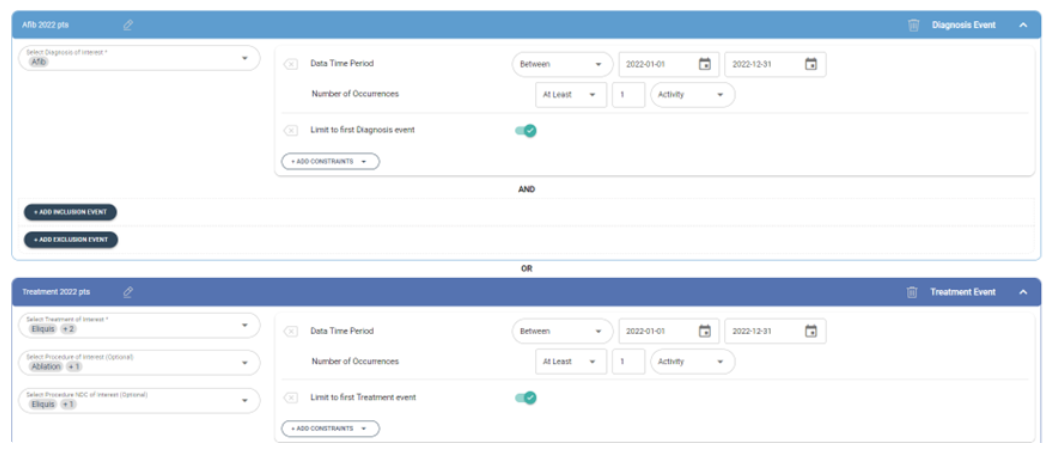
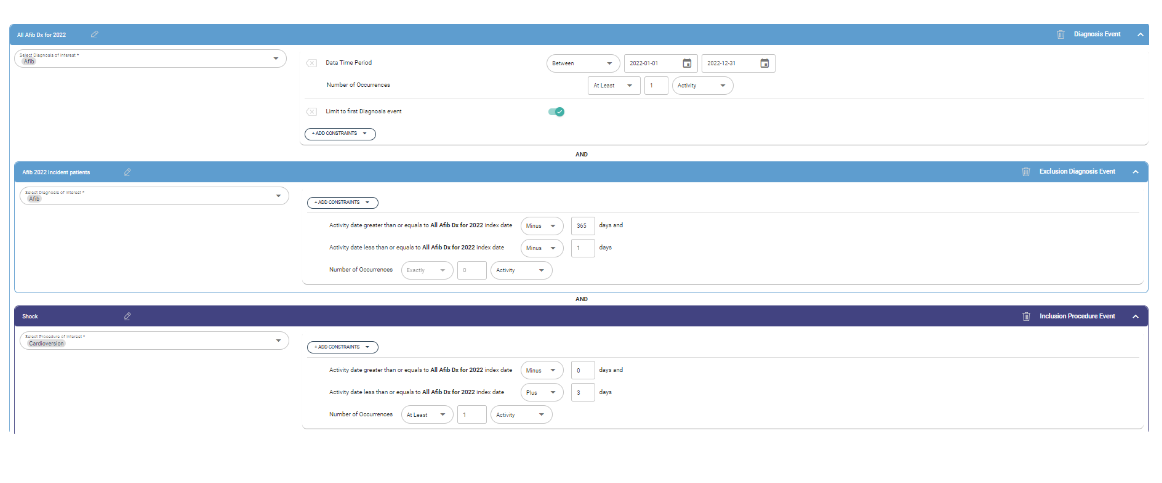
Scenario1: Identify Patients with at least Atrial fibrillation in 2022.
Add Diagnosis event, select Atrial fibrillation diagnosis from Diagnosis of Interest, filter for 2022 ‘data time period from ‘add constraints’ list, distinct number of occurrences based on claim_id and activity date, filter for limit to first diagnosis to get minimum date in 2022. We can evaluate number of occurrences among activity or claim.
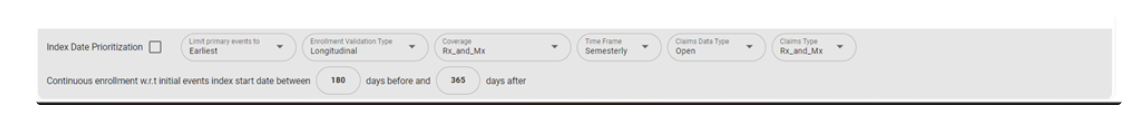
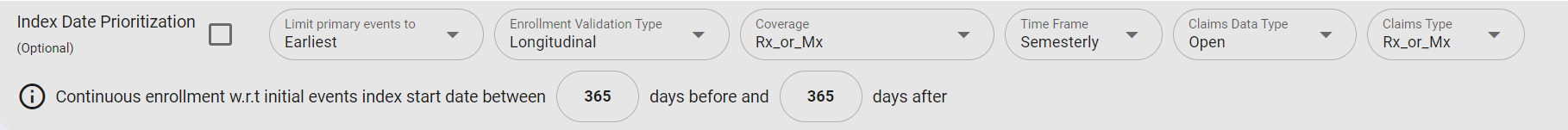
Case1: Continuous Enrollment
Lookback 180 and look forward 365 RX&MX Semesterly Continuous Enrollment based on Index date. Let’s assume, patient index date 2022-01-31 then LB date is 2021-08-04 and LF date is 2023-01-31. This means patients should have at least one Rx&Mx claim on semesterly basis from 2021-H2, 2022-H1, 2022-H2, 2023-H1.
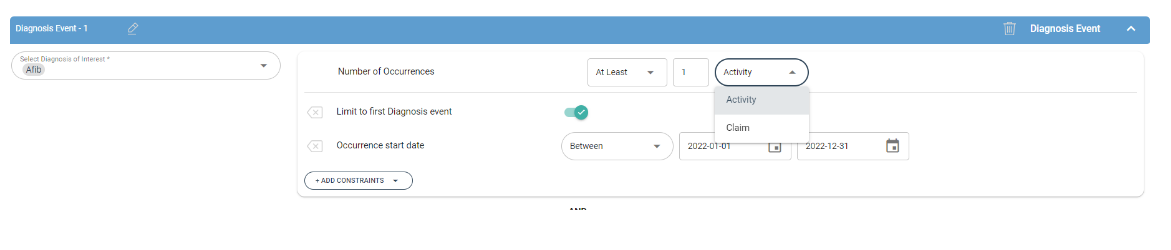
Scenario2: Identify Atrial Fibrillation New Patients in 2022
Add Diagnosis event, select Atrial fibrillation diagnosis from Diagnosis of Interest, distinct number of occurrences based on claim_id and activity date, filter for limit to first diagnosis to get minimum date from 2018 to latest data. Filter the minimum date to 2022.
2.Two Individual Events
Scenario1: Assume to identify patients in 2022 based on Atrial Fibrillation or Treatment / Procedure
Add Diagnosis event - Select Atrial fibrillation diagnosis from Diagnosis of Interest, filter for 2022 ‘data time period from ‘add constraints’ list, distinct number of occurrences based on claim_id and activity date, filter for limit to first diagnosis to get minimum date in 2022.
Add Treatment/Procedure event -
Treatment of Interest (NDC) values / Select Procedure of Interest (Procedure, HCPCS, CPT), filter for 2022 data time period from ‘add constraints’ list, distinct number of occurrences based on claim_id and activity date, filter for limit to first activity to get minimum date in 2022.
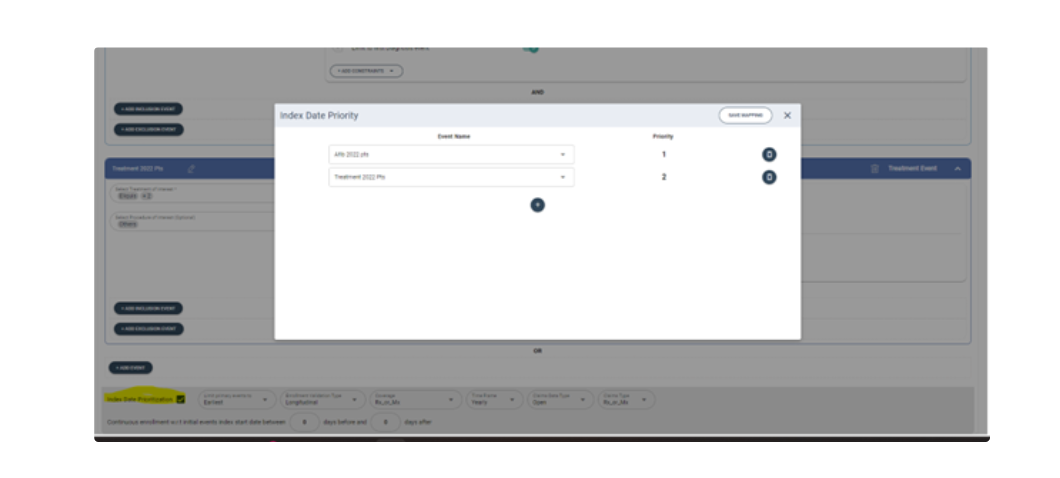
Index Date Prioritization
Scenario1
The default method will union diagnosis and treatment events to Identify minimum date. Example- If diagnosis index date is 2022-02-01 and treatment index date is 2022-01-31 then 2022-01-31 is considered as index date. We can customize index date selection based on index Date prioritization option(highlighted). In this customization example, we are prioritizing Afib index dates over treatment date so the index date will be 2022-02-01.
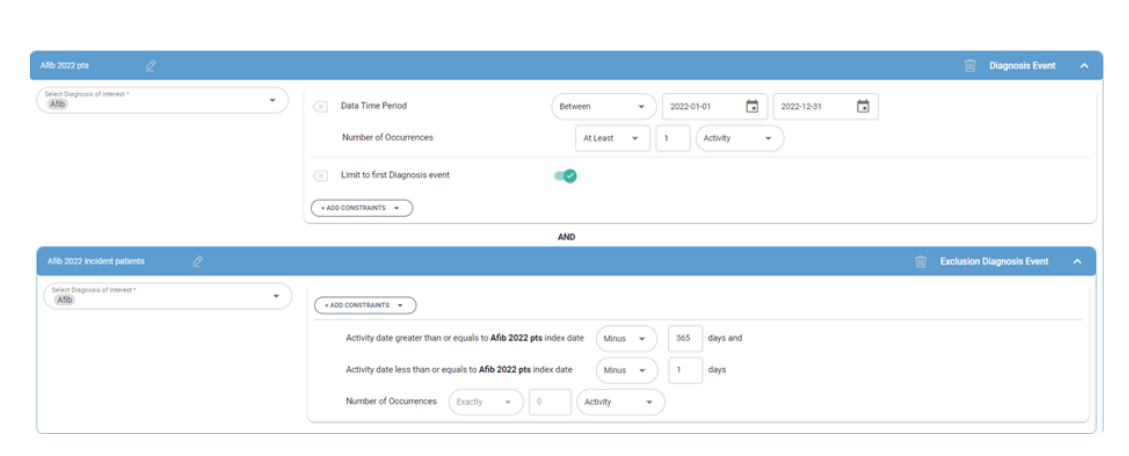
3.Related Events
Scenario1: Identify Atrial Fibrillation Incidence Patients in 2022
Main Event - Add Diagnosis event, select Atrial fibrillation diagnosis from Diagnosis of Interest, filter for 2022 ‘data time period from ‘add constraints’ list, distinct number of occurrences based on claim_id and activity date, filter for limit to first diagnosis to get minimum date in 2022.
Related Exclusion Event – no claim of Afib diagnosis 365 days prior to 2022 index date.
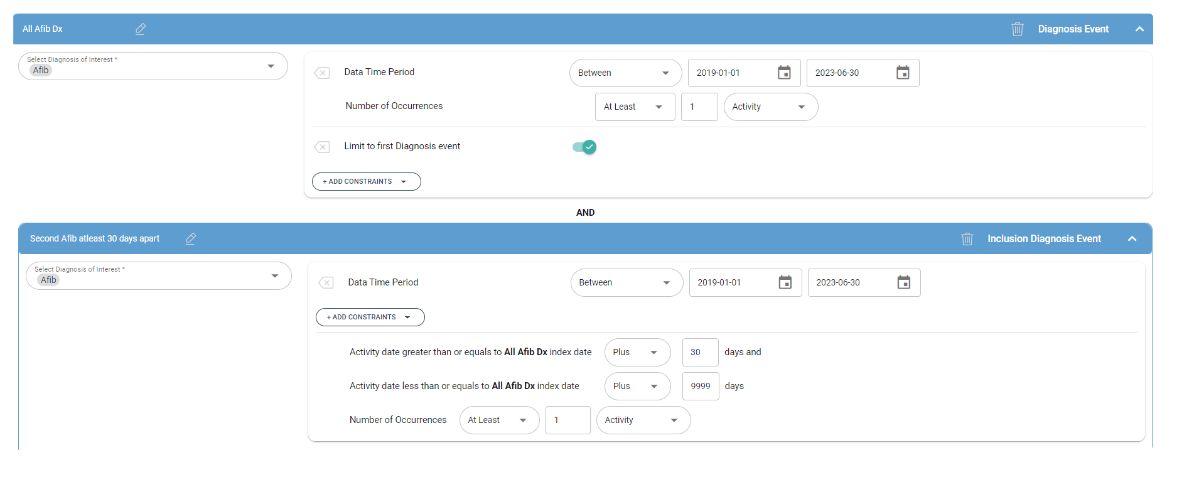
Scenario2: Identify Two Afib Diagnosis claims at least 30 days apart in a specific study period.
Main Event - Add Diagnosis event, select Afib diagnosis from Diagnosis of Interest, filter for 2019-01-01 to 2022-06-30 ‘data time period from ‘add constraints’ list, distinct number of occurrences based on claim_id and activity date, filter for limit to first diagnosis to get minimum date.
Related Inclusion Event – Second Afib claim 30 days apart from first Afib claim. In this example, the second Afib claim should be greater than equals to first Afib claim Plus 30 days and second Afib claim should be less than equals to first Afib claim Plus 9999.
Scenario3: Identify Atrial Fibrillation Incidence Patients in 2022 and Shock within Three days of Atrial Fibrillation Index date.
Main Event - Add Diagnosis event, select Atrial fibrillation diagnosis from Diagnosis of Interest, filter for 2022 ‘data time period from ‘add constraints’ list, distinct number of occurrences based on claim_id and activity date, filter for limit to first diagnosis to get minimum date in 2022.
Related Exclusion Event – no claim of Afib diagnosis 365 prior to 2022 index date.
Related Inclusion Event - Cardioversion procedure with in three days of index date.
4.Individual Event Constraints Mandatory, Select Event of interest Codes i.e., Diagnosis / Procedure / Treatment / Surgery
Optional, Data Time Period to filter respective event data on specific study period.
Mandatory, Number of Occurrences –
Distinct count of Claim id and Activity date
Count of Claim id and Activity date
Optional, First Event – Limit of minimum activity date and order by claim id.
Optional, Occurrence start date – primarily leverage to filter on minimum activity date
Optional, Gender – limit any specific gender.
Optional, Age at occurrence – limit to any specific age
Optional, Provider Specialty – limit to any specific specialty of interest patients.
Related Event Constraints
Mandatory, Select Event of interest Codes i.e., Diagnosis / Procedure / Treatment / Surgery
Optional, Data Time Period to filter respective event data on specific study period.
Optional, First Event – Limit of minimum activity date and order by claim id.
Optional, Occurrence start date – primarily leverage to filter on minimum activity date
Optional, Gender – limit any specific gender.
Optional, Age at occurrence – limit to any specific age
Optional, Provider Specialty – limit to any specific specialty of interest patients
Related Event Activity Date greater than or equals to Main Event Index date Minus/Plus 9999 days and Related Event Activity Date greater than or equals to Main Event Index date Plus/Minus 9999 days
Mandatory, Number of Occurrences –
Distinct count of Claim id and Activity date
Count of Claim id and Activity date
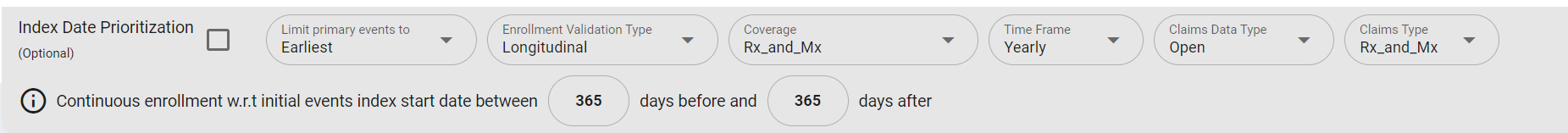
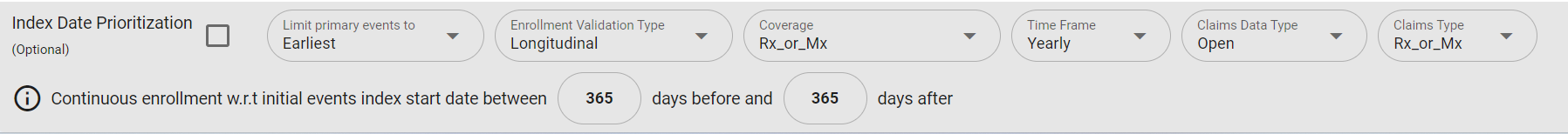
5.Continuous Enrollment Longitudinal – Symphony Symphony (enrollment proxy is created based on yearly/semesterly claims activity (both approved & rejected claims are considered for activity)). Enrollment Validation Type - Longitudinal is with respective to Index date.
Coverage – Users can select based on Rx or Mx, Rx_and_Mx etc.
Time Frame – Yearly & Semesterly
Yearly (Rx_and_Mx)
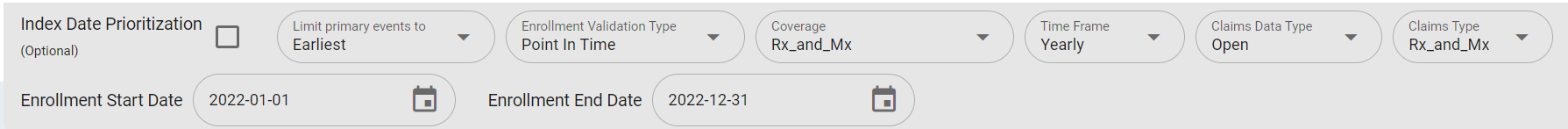
At least one activity of pharmacy AND medical claim in a calendar year is required to be considered as complete enrollment in that calendar year. Example: 1. Enrollment Validation Type = Point In Time Input condition - Enrollment start date = 2022-01-01 and Enrollment end date = 2022-12-31 Backend implementation - Patient is required to have pharmacy activity AND medical activity calendar year 2022.
- Enrollment Validation Type = Longitudinal Input condition - Patient has Index date in March 2022 and is required to have Continuous enrollment of 365 days before and 365 days after Index date. Backend implementation - Continuous enrollment will be determined by requiring a patient to have pharmacy AND medical activity in calendar year 2022, 2021 (365 days before) and 2023 (365 days after) time period.
Yearly (Rx_or_Mx)
At least one activity of pharmacy OR medical claim in a calendar year is required to be considered as complete enrollment in that calendar year. Example: 1. Enrollment Validation Type = Point In Time Input condition - Enrollment start date = 2022-01-01 and Enrollment end date = 2022-12-31 Backend implementation - Patient is required to have pharmacy activity OR medical activity calendar year 2022.
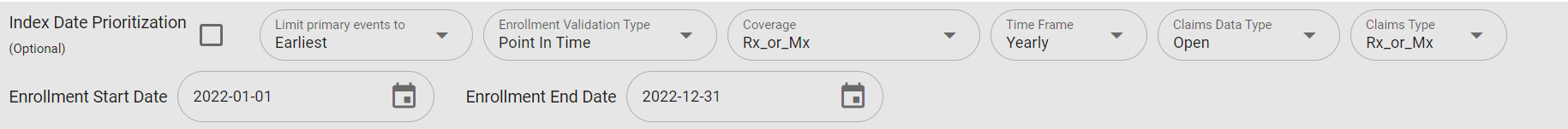
- Enrollment Validation Type = Longitudinal Input condition - Patient has Index date in March 2022 and is required to have Continuous enrollment of 365 days before and 365 days after Index date. Backend implementation - Continuous enrollment will be determined by requiring a patient to have pharmacy OR medical activity in calendar year 2022, 2021 (365 days before) and 2023 (365 days after) time period.
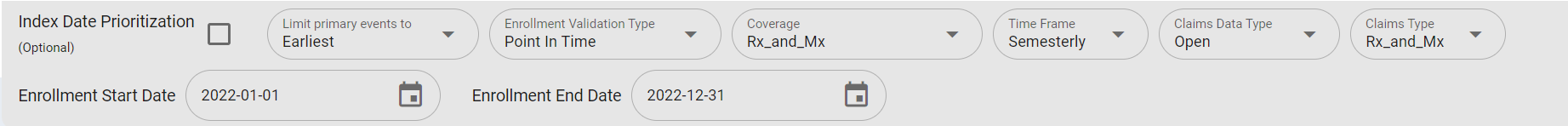
Semesterly (Rx_and_Mx) At least one activity of pharmacy AND medical claim in a semester (Jan-Jun, Jul-Dec) is required to be considered as complete enrollment in that semester. Example: 1. Enrollment Validation Type = Point In Time Input condition - Enrollment start date = 2022-01-01 and Enrollment end date = 2022-12-31 Backend implementation - Patient is required to have pharmacy activity AND medical activity in Jan 2022 - Jun 2022 period AND patient is required to have pharmacy activity AND medical activity in Jul 2022 - Dec 2022 time period.
- Enrollment Validation Type = Longitudinal Input condition - Patient has Index date in Jan 2022 and is required to have Continuous enrollment of 365 days before and 365 days after Index date. Backend implementation - Continuous enrollment will be determined by requiring a patient to have pharmacy AND medical activity in in each of the two semesters of Jan 2021 - Jun 2021 and Jul 2021 - Dec 2021 (365 days before) and in each of the two semesters of Jan 2023 - Jun 2023 and Jul 2023 - Dec 2023 (365 days after) time period.
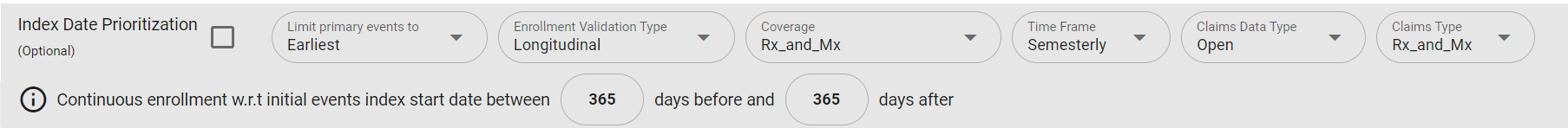
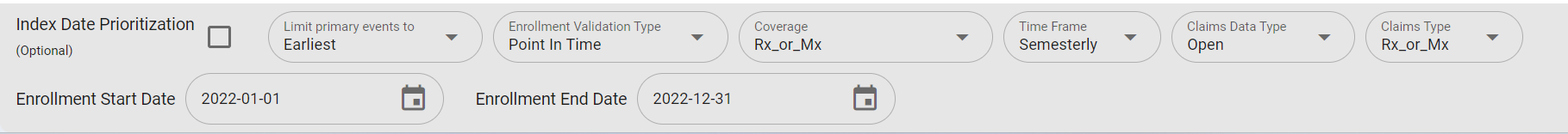
Semesterly (Rx_or_Mx) At least one activity of pharmacy OR medical claim in a semester (Jan-Jun, Jul-Dec) is required to be considered as complete enrollment in that semester. Example: 1. Enrollment Validation Type = Point In Time Input condition - Enrollment start date = 2022-01-01 and Enrollment end date = 2022-12-31 Backend implementation - Patient is required to have pharmacy activity OR medical activity in Jan 2022 - Jun 2022 period AND patient is required to have pharmacy activity OR medical activity in Jul 2022 - Dec 2022 time period.
- Enrollment Validation Type = Longitudinal Input condition -Patient has Index date in Jan 2022 and is required to have Continuous enrollment of 365 days before and 365 days after Index date. Backend implementation - Continuous enrollment will be determined by requiring a patient to have pharmacy OR medical activity in each of the two semesters of Jan 2021 - Jun 2021 and Jul 2021 - Dec 2021 (365 days before) and in each of the two semesters of Jan 2023 - Jun 2023 and Jul 2023 - Dec 2023 (365 days after) time period.
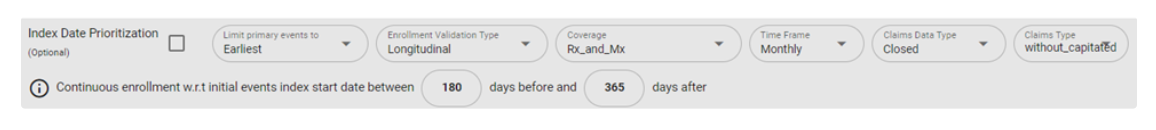
Longitudinal – Marketscan / Komodo/CMS
Enrollment Validation Type - Longitudinal is with respective to Index date.
Coverage – Users can select based on Rx_and_Mx coverage.
Time Frame –
a. Monthly Enrollment
b. For Komodo – We are considering if patient has at least one day of enrollment in a month. Example- if patient enrollment start date is Jan-15th we are considering it from Jan 1st
Claims Type - For Marketscan we have 2 Claim type – With_capitated and Without_Capitated
Continuous enrollment w.r.t initial events index start date between xx(180) days before and xx(365) days after
Example- Lookback 180 and look forward 365 RX&MX Monthly Continuous Enrollment based on Index date. Let’s assume, patient index date 2022-01-31 then LB date is 2021-08-04 and LF date is 2023-01-31. This means patients should be continuous enrolled for Rx&Mx on monthly basis from 2021-08-04 to 2023-01-31.
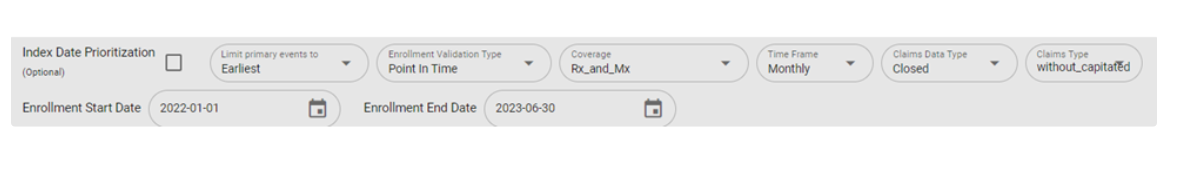
Point In Time – Marketscan / Komodo/CMS
Enrollment Validation Type – Point In Time irrespective of Index date.
Coverage – Users can select based on Rx_and_Mx coverage.
Time Frame –
a. Monthly Enrollment
b. For Komodo – We are considering if patient has at least one day of enrollment in a month. Example- if patient enrollment start date is Jan-15th we are considering it from Jan 1st.
Claims Type - For Marketscan we have 2 Claim type – With_capitated and Without_Capitated
Enrollment Start Date and Enrollment End Date
a. Enrollment Start Date 2022-01-01 and Enrollment End Date 2023-06-30 on Monthly selection. This means patients should be continuously enrolled from 2022-01-01 to 2023-06-30.